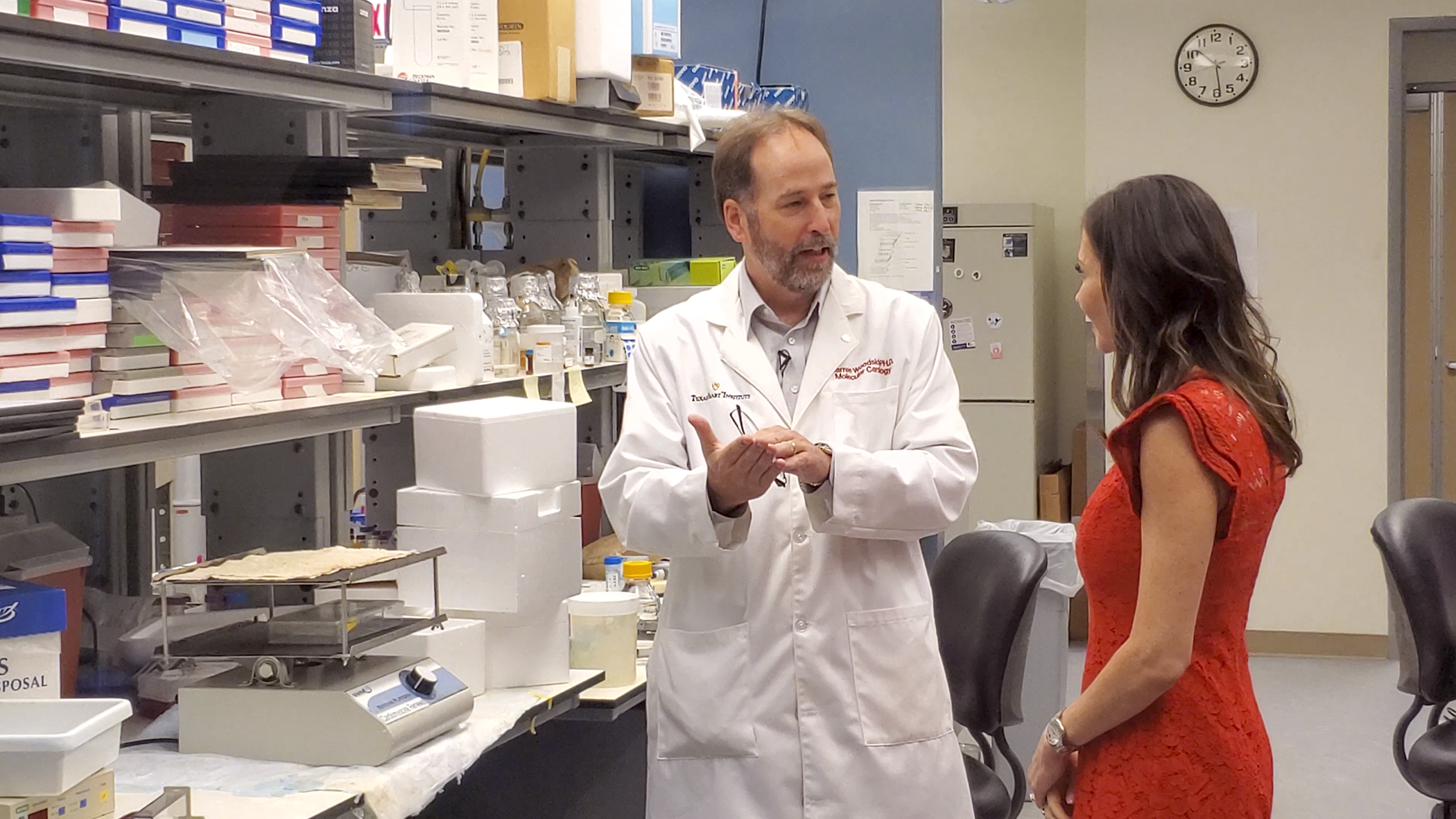
Scientists and researchers in Texas Heart Institute’s Molecular Cardiology Research Laboratories (MCRL) are ideally positioned to discover and develop new cardiovascular drugs. The team approaches clinical challenges using a two-pronged approach: They combine their detailed insights into the molecular mechanisms of heart and vascular diseases with the drug-discovery expertise they honed while working in the pharmaceutical industry.
By discovering novel drug compounds and then developing promising candidates, the team produces unique small-molecule drugs and compounds that can improve the diagnosis, treatment, and prevention of cardiovascular disease. MCRL investigators collaborate across departments, disciplines, and research institutions to identify unmet clinical needs and devise new treatment options for patients.
Small-molecule Drug Completes Phase I Trial
An NIH-sponsored Phase I clinical trial in healthy volunteers was completed that evaluated the safety and bioavailability of the first small-molecule drug developed at THI to enter human testing. The drug, a novel integrin activator, was found to be safe and well-tolerated, with no serious adverse events detected. It can be taken by mouth (orally bioavailable); two 50-mg soft gel capsules yielded the targeted optimal pharmacokinetic dose.
In preclinical studies, the drug has been shown to enhance stem cell transplant, as well as to improve the body’s immune response to vaccines (see below) and cancer immunotherapies. The results from this Phase I study will be used to support future trials of the drug for these clinical indications.
Enhancing Vaccine Immune Responses
A strong correlation exists between certain infectious diseases and cardiovascular complications. These diseases include influenza, COVID-19, and Chagas disease. In the case of influenza and COVID, elderly people are particularly susceptible, as the ability of the immune system to respond to infections becomes compromised with age. Although vaccines have proven effective in greatly reducing the risk of infection and serious illness in the general population, the immune response to many vaccines, including those targeting influenza and COVID-19, is not as robust in elderly or immunocompromised patients.
MCRL investigators and their collaborators have discovered a simple way to enhance the immune response to vaccines against infections linked to cardiovascular disease. They have developed a drug that has proven safe and orally available in clinical trials (see above) and that has been shown in preclinical models to enhance the immune response to influenza, COVID-19, and Chagas vaccines when dosed systemically, separate from the vaccine.
This suggests that the drug could be combined with numerous vaccines that have already been formulated and stockpiled. A proof-of-concept study with an experimental Chagas vaccine was published this year in the journal Vaccines. Unlike flu and COVID-19, no Chagas vaccine is currently approved for clinical use, and no adjuvant had yet proved effective in enhancing the response to the particular vaccine used in this study.
UNIQUE DISCOVERY
“Although Chagas is not an overly common ailment, it is a very serious disease that can cause heart failure and stroke with lethal consequences. The study speaks to the power of multidisciplinary scientific collaboration and would not have been possible without the efforts of the talented individuals at 7 Hills Pharma and UTMB.” – Darren G. Woodside, PhD Vice President for Research
Anti-inflammatory Drug with Reduced Cardiovascular Toxicities
Inhibiting the signaling pathways of cellular receptors involved in physiological responses is a common approach to treat inflammatory diseases. However, drugs targeting kinase pathways are notoriously non-selective, leading to unwanted side effects that often include cardiovascular toxicities, or damage to the heart and blood vessels. MCRL investigators have identified small-molecule compounds that can inhibit a kinase called “Syk” that binds to the cytoplasmic tails of a class of cell adhesion receptors called integrins. This interaction is key to triggering an inflammatory response.
The compounds inhibit signaling by Syk and decrease expression of inflammatory cytokines by leukocytes, a type of immune cell. This discovery is unique in that the drugs do not bind at the conserved kinase binding sites typically targeted by the pharmaceutical industry and thus show better selectivity—or the ability to produce the intended effect—and, therefore, fewer potential toxicities. This work was published in Frontiers in Immunology.
Explore our new Digital Annual Report or read the report in a Flipbook or Mobile/Tablet view.