Study Shows Selection of Coronary Stenting versus Bypass Surgery for Coronary Artery Disease Differs by Race and Ethnicity

Progress made in African American Patients, but disparity remains.
Clinical researchers at the Texas Heart Institute have taken an in-depth look at racial and ethnic differences in the outcomes of two common treatments for coronary artery disease (CAD).
The study found that, compared with White patients, African American patients were more likely to undergo percutaneous coronary intervention procedures (PCI or “stenting”) instead of open-heart, coronary artery bypass graft surgery (CABG), whereas Hispanic and Asian patients were less likely.
After adjustment for medical risks, African American patients who underwent CABG had worse outcomes. African American and Hispanic patients were more likely to die in the hospital after CABG but not after PCI. In addition, costs were significantly higher for African American, Hispanic, and Asian patients than for White patients, regardless of whether they underwent PCI or CABG.
“It is becoming increasingly evident that we are not doing enough to narrow the gaps in care provided to various population groups in the US. The difference in outcomes between Blacks, Hispanics, and Whites may be in part due to differences in biology, but it is overwhelmingly more likely to be related to socioeconomic factors. We know that better access to care and higher income markedly improves health outcomes; the zip code where you live can be more predictive of life expectancy than your race. This research by our own THI investigators is a welcome addition that brings attention to this matter,” said Alexander Postalian, MD, Interventional Cardiologist at the Texas Heart Institute.
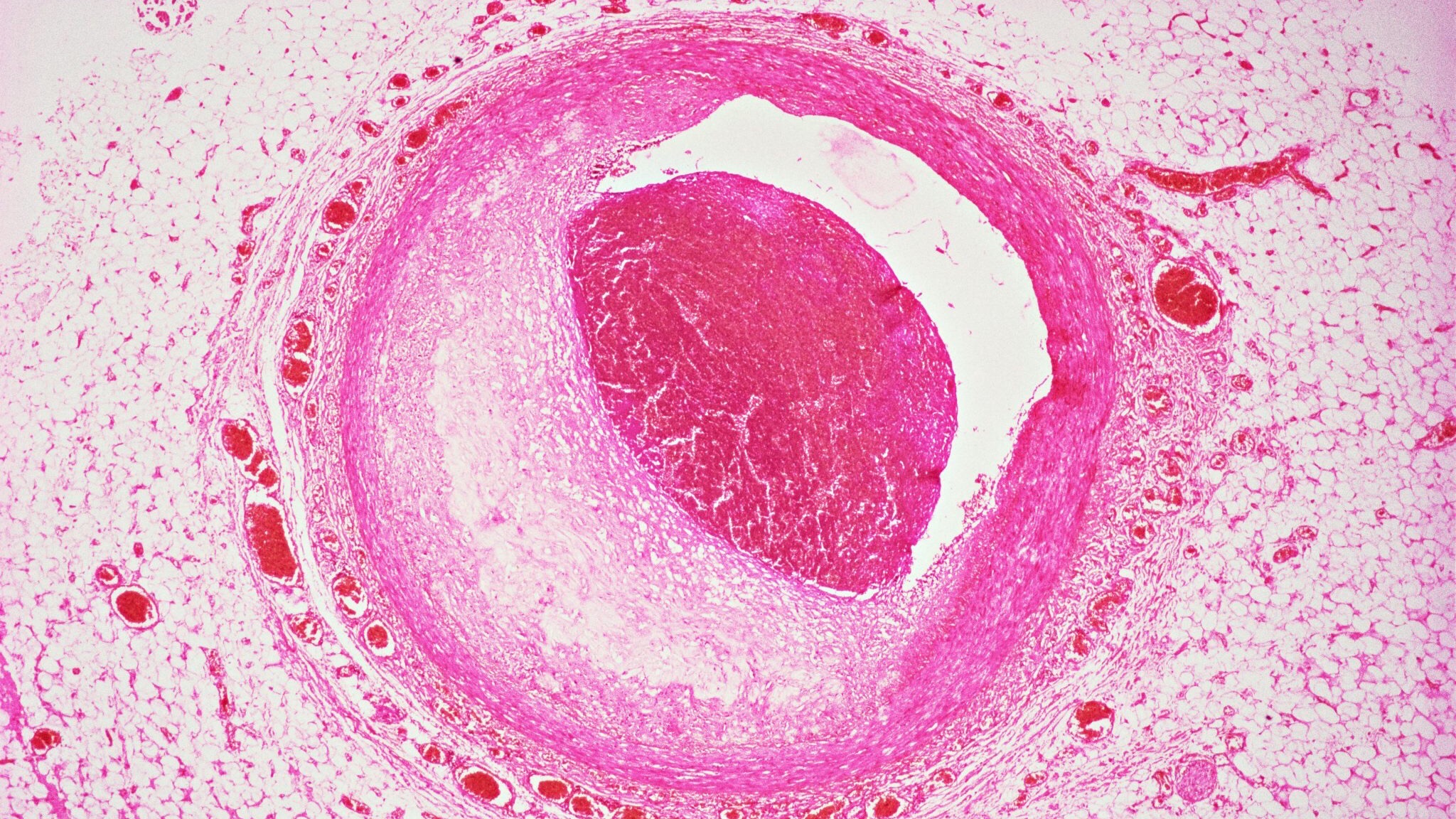
CAD is the leading cause of death for both men and women across most racial and ethnic groups. CAD develops when the coronary arteries that supply oxygen-rich blood to the heart become clogged by the buildup of a waxy, fatty substance called plaque, potentially slowing or stopping blood flow enough to cause a heart attack.
Advanced CAD is usually treated with either PCI or CABG. PCI is a minimally invasive surgical procedure in which a catheter is inserted into a large vein or artery and then threaded into the blocked coronary artery. The catheter tip has a small balloon that can be inflated at the blockage site to flatten the plaque against the artery wall. A miniature mesh-like metal tube, or stent, can be inserted to keep the vessel open and prevent the artery from collapsing. CABG is an open-heart operation in which a segment of vein or artery (usually taken from the leg, arm, or chest) is used to route blood flow around the blockage.
Race, ethnicity, and socioeconomic status are known to affect both access to care and the results of care for patients with CAD. For example, a 2001 study found that African American patients were less likely than White patients to undergo either CABG or PCI. However, studying African American and White patients captures only part of the story. US racial/ethnic demographics have shifted in the past 20 years, including sizeable growth in Hispanic and Asian populations—who have often been excluded from studies because of low patient volumes. All of these groups must be analyzed separately if health care providers are to understand how racial and ethnic differences affect cardiac surgical care.
To that end, THI researchers analyzed a large dataset from a nationwide registry, the National Inpatient Sample (NIS), to map trends and outcomes of PCI and CABG by race and ethnicity. The study covered a 15-year period from 2002 to 2017 and focused on the four most common racial and ethnic categories in the NIS: White, African American, Hispanic, and Asian. The researchers were interested in how race and ethnicity might affect the choice of treatment (PCI or CABG), survival, and hospital costs.
The NIS dataset included 7.2 million PCI patients and 2.4 million CABG patients. Of these, 83% were White, 8% were African American, 7% were Hispanic, and 2% were Asian. Although the White patients were generally older, they were more likely to have Medicare insurance coverage and less likely to have other medical problems.
The authors suggested three possible reasons for the CAD treatment and outcomes differences between racial and ethnic groups:
- Patient medical factors – the African American patients in the study were more likely to have additional illnesses and medical conditions than the other groups; they could also have had a form of CAD that responds better to PCI than to CABG, which might have influenced their choice of procedure.
- Unconscious biases and trust factors – studies show that minorities are generally more likely to undergo less-invasive treatment; improving racial and ethnic diversity among physicians might offset this trend, as patients tend to be more open to advice from racially concordant health care providers. Even so, patients often base their treatment choice on social factors, such as knowing someone who underwent the procedure or having a support network; educational level also can influence treatment decisions.
- Socioeconomic factors – African American individuals more frequently receive care at hospitals that have higher mortality rates due to geographic location (especially so-called “safety-net” hospital locations), referral patterns, and ambulance routes.
Interestingly, comparing the current study with the earlier 2001 report revealed that African American and White patients have become more similar in terms of choosing a procedure. A possible reason for this is the insurance expansion that happened after the passage of the Affordable Care Act in 2010. Cardiac surgery volumes increased in Medicaid-expansion states, strongly suggesting that insurance status affects which surgical options are available.
One limitation of the study is that the NIS registry did not provide any information about the anatomy of the underlying CAD, which could have been an important factor in choosing between PCI and CABG. Nonetheless, this large database did provide 15 years of nationally representative, real-world data.
Said Ravi Ghanta, MD, member of the Professional Staff at THI, Associate Professor of Cardiothoracic Surgery at Baylor College of Medicine, and lead investigator of this study, “Considering the persistent differences in treatment choice and treatment outcomes confirmed by our study, further research is needed to identify the root causes of these differences—especially for our African American patients, who continue to be at risk. Our long-term goal should be to improve outcomes in at-risk groups.”
Read Report
Zea-Vera R, Asokan S, Shah RM, Ryan CT, Chatterjee S, Wall MJ Jr, Coselli JS, Rosengart TK, Kayani WT, Jneid H, Ghanta RK. Racial/ethnic differences persist in treatment choice and outcomes in isolated intervention for coronary artery disease. J Thorac Cardiovasc Surg. 2022; doi: https://doi.org/10.1016/j.jtcvs.2022.01.034.
News Story By Jeanie F. Woodruff, BS, ELS


